Health
- Details
- Health
A 12-member ethics panel convened by the United Nations health agency today reached "unanimous consensus" that it is ethical to treat Ebola patients with experimental drugs to counter the largest, most severe and most complex outbreak of the virus in history.
"There was unanimous agreement among the experts that in the special circumstances of this Ebola outbreak it is ethical to offer unregistered interventions as potential treatments or prevention," UN World Health Organization (WHO) Assistant Director-General for Health Systems and Innovation, Marie-Paule Kieny, told a press conference in Geneva.
The WHO, in a statement on the outcome of the two-day Emergency Committee of experts, said that "over the past decade, research efforts have been invested into developing drugs and vaccines for Ebola virus disease. Some of these have shown promising results in the laboratory, but they have not yet been evaluated for safety and efficacy in human beings."
Dr. Kieny said several of these treatments have proven to be very effective in non-human primates – monkeys – but none have been tested on humans. Currently, there are no licensed treatments or vaccines for Ebola.
At the UN Headquarters in New York, Secretary-General Ban Ki-moon designated David Nabarro as the Senior UN System Coordinator for Ebola Virus Disease. In a press encounter, he called on the international community to respond urgently to the shortage of doctors, nurses and equipment, including protective clothing and isolation tents, saying "We need all hands on deck."
He also made an appeal to avoid panic and fear, stressing that "Ebola has been successfully brought under control elsewhere, and we can do it here, too."
Meanwhile, WHO said in its latest update of the current Ebola outbreak in West Africa that between 7 and 9 August, a total of 69 new cases and 52 deaths were reported from Guinea, Liberia, Nigeria, and Sierra Leone, bringing the total numbers of cases to 1,848 with 1,013 deaths.
WHO has posted Ebola response videos on YouTube and is also seeking to counter the "many barriers stand in the way of rapid containment."
"Fear is proving to be the most difficult barrier to overcome," WHO said. "Fear causes contacts of cases to escape from the surveillance system, families to hide symptomatic loved ones or take them to traditional healers, and patients to flee treatment centres."
"Fear, and the hostility it can feed, have threatened the security of national and international response teams," the UN agency added.
WHO has declared the current Ebola outbreak an international public health emergency. The large number of people affected by the 2014 West African outbreak, and the high case-fatality rate have prompted calls to use investigational medical interventions to try to save the lives of patients and to curb the epidemic.
In this context, WHO yesterday convened a virtual consultation of researchers, ethicists, and patient safety advocates from around the world to consider and assess the ethics surrounding the use of therapies when safety is unproven, ethics governing priority setting for access to these therapies and principles for fair distribution.
"Ethical criteria must guide the provision of such interventions," WHO said. "These include transparency about all aspects of care, informed consent, freedom of choice, confidentiality, respect for the person, preservation of dignity and involvement of the community."
The Ebola virus is highly contagious, but is not airborne, according to UN experts. Transmission requires close contact with the bodily fluids of an infected person, as can occur during health-care procedures, home care, or traditional burial practices, which involve the close contact of family members and friends with bodies.
The incubation period ranges from 2 to 21 days, but patients become contagious only after the onset of symptoms. As symptoms worsen, the ability to transmit the virus increases. As a result, patients are usually most likely to infect others at a severe stage of the disease, when they are visibly, and physically, too ill to travel.
- Details
- Ngwa Bertrand
- Hits: 2861
- Details
- Health
Nigerian officials now say one new Ebola case was diagnosed over the weekend, raising the country's total to 10 confirmed cases, while Ivory Coast banned air travel from West African nations heavily hit by the virus. Ever since Patrick Sawyer, a Liberian-American financial consultant, flew into Lagos from Monrovia about three weeks ago, the number of new Ebola cases has slowly grown and the number of people who may have been exposed is growing. Government officials are now monitoring 177 people for symptoms of the disease. Over the weekend, a 10th person who had an apparent connection with Sawyer was diagnosed with Ebola, said Onyebuchi Chukwu, Nigerian Minister of Health. "It was one of the nurses that were primary contacts when he got ill. We then brought her into isolation and we just tested her over the weekend and she tested positive,'
Of the 10 cases of Ebola in Nigeria, there have been two deaths: Sawyer and a nurse who treated him when he first arrived in Lagos. The other eight cases are people who also had direct contact with Sawyer. Ebola has killed 961 people since the outbreak began early this year, with all but two deaths occurring in Liberia, Guinea and Sierra Leone. Ebola is one of the world's most deadly diseases, with no known vaccine or cure. The Zaire strain - the one currently spreading through West Africa - can kill up to 90 percent of sufferers, although in the latest outbreak the death toll has been around 55 percent. Reports that experimental drugs have had success in treating American and European health workers and missionaries who contracted the disease in West Africa have prompted many Nigerians to demand access to the drugs in case it spreads further. Nigeria is actually, as of now, reaching out to various laboratories, various governments, including the U.S.A. government to see how these untried ... drugs that seem to hold some hope could also be deployed in Nigeria. We're in touch. The World Health Organization said it expects a vaccine to be developed by 2015, but currently there is no known cure.
Nigerian President Goodluck Jonathan Friday pledged $11.7 million dollars to try to stop the spread in Nigeria and $3.5 million to help other countries fight the disease. So far in Nigeria, the disease has not spread out of Lagos, a megacity of 21 million people that is often called the 'heartbeat' of the Nigerian economy. As Nigeria joins the group of West African nations battling an Ebola outbreak, other countries are taking stronger measures to prevent the virus from entering its borders. In Ivory Coast, the government has banned, until further notice, all passenger flights into the country from Liberia, Guinea or Seirra Leone, the three countries hardest hit by the virus.Ivory Coast has not reported any cases of Ebola and government spokesman Bruno Kone said they want to keep it that way.The government said in addition to the ban on flights, authorities at the Abidjan airport will be screening all arriving passengers for fever, using infrared thermometers. Fever can be one of the early symptoms of Ebola.It can take up to 21 days for symptoms to appear, and once they do, a person is contagious. Other people can catch the disease by coming into contact with the sick person's bodily fluids.
While Ivory Coast shares land borders with two of the four affected countries - Liberia and Guinea - Health Minister Dr. Raymonde Goudou Coffie said it doesn't make sense to shut those borders. Coffie said the borders are very porous, and even if they close the official borders, people know other ways across.Instead, she said, health officials have worked on educating villages and local leaders to have them refer new arrivals to health authorities Liberia closed its land border with Ivory Coast last week in an attempt to prevent the spread of the virus.Ivory Coast's defense minister said in "recent days," border authorities have already repatriated 'nearly 100 people' who have tried to cross illegally from Guinea or Liberia.The Ivory Coast government said it continues to train health workers and will be holding a simulation drill later this week for first responders. In Malawi, health authorities said the government was taking measures to prevent the spread of the Ebola virus into the country, including airport screenings of international passengers, critics said they weren't doing enough. Charles Mwansambo, director of health services in the Ministry of Health, told journalists in Lilongwe that the government was screening international passengers at the airports, and had set up quarantine centers at Kamuzu International Airport in the capital, Lilongwe, and Chileka Airport, in the commercial capital of Blantyre. However, critics said that medical workers needed urgent training on how to handle an infected person, lacked specialized equipment for containing the virus and could improve public education efforts. Ministry of Health officials said the airport screenings are currently done to those passengers from West African countries hit hardest by the Ebola virus - Guinea, Liberia, Nigeria and Sierra Leone. Mwansambo said, "I want to assure the members of the general public not to panic because Ebola is spread by direct contact with bodily fluids like blood, saliva and urine. And chances of Malawians going to West Africa and getting in touch with these bodily fluids are very minimal."
Juliana Lunguzi, chairwoman of Malawi's Parliamentary Committee on Health, criticized his comments, saying there is no logic in telling people not to panic when the situation on the ground shows the government is doing nothing to prevent the outbreak. Lunguzi, who is also a nurse, said her committee will soon summon government authorities to explain their readiness in terms of medical equipment for combating the possible spread of Ebola into the country. Jonathan Gama, chairman of the Human Resources for Health coalition of health professionals in Malawi, said Malawi is not in any way ready to contain the virus. Gama cited inadequate medical equipment, protective wear and orientation for health workers as among the signs of the country's unpreparedness."What we are suggesting is that the health workers should be trained and after training them there should be procurement of resources as Ebola demands, so that when Ebola incidences appear in Malawi we should not be taken by surprise”.
- Details
- Ngwa Bertrand
- Hits: 3437
- Details
- Health
Health workers in West Africa appealed on Wednesday for urgent help in controlling the world’s worst Ebola outbreak as the death toll climbed to 932 and Liberia declared a state of emergency.
“The government and people of Liberia require extraordinary measures for the very survival of our state and for the protection of the lives of our people,” Liberian President Ellen Johnson-Sirleaf said in an official statement. The state of emergency was for 90 days, effective Wednesday.
Liberia also shut a major hospital where several staff were infected, including a Spanish priest.
The World Health Organisation (WHO) said it would ask medical ethics experts to explore emergency use of experimental treatments to tackle the highly contagious disease after a trial drug was given to two U.S. charity workers infected in Liberia.
With West Africa’s rudimentary healthcare systems swamped, 45 new deaths from Ebola were reported in the three days to Aug. 4, the WHO said. Liberia and Sierra Leone have deployed troops in the worst-hit areas in their remote border region to try to stem the spread of the virus, for which there is no known cure.
WHO experts began a two-day crisis meeting in Geneva to discuss whether the epidemic constitutes a “Public Health Emergency of International Concern” and to consider steps to help overstretched emergency organizations.
“This outbreak is unprecedented and out of control,” said Walter Lorenzi, head of medical charity Medecins Sans Frontieres (MSF) in Sierra Leone. “We have a desperate need for other actors on the ground, not in offices or in meetings, but with their rubber gloves on, in the field.”
International alarm at the diffusion of the virus increased when a U.S. citizen, Patrick Sawyer, died in Nigeria last month after flying there from Liberia. Authorities said on Wednesday that a Nigerian nurse who had treated Sawyer had also died of Ebola, and five other people were being treated in an isolation ward in Lagos, Africa’s largest city.
With doctors on strike, Lagos health commissioner Jide Idris said volunteers were urgently needed to track 70 people who came into contact with Sawyer. Only 27 have so far been traced.
“We have a national emergency, indeed the world is at risk,” Nigerian Health Minister Onyebuchi Chukwu said after a weekly cabinet meeting in Abuja. “Nobody is immune. The experience in Nigeria has alerted the world that it takes just one individual to travel by air to a place to begin an outbreak.”
U.S. health regulators authorized an Ebola diagnostic test developed by the Pentagon for use abroad on military personnel, aid workers and emergency responders in laboratories designated to help contain the outbreak.
The test is designed for use on people who have symptoms of Ebola infection, are at risk or may have been exposed. It can take as long as 21 days for symptoms to appear after infection.
In Saudi Arabia, a man suspected of contracting Ebola during a recent business trip to Sierra Leone also died early on Wednesday in Jeddah, the Health Ministry said. Saudi Arabia has already suspended pilgrimage visas from West African countries, which could prevent those hoping to visit Mecca for the haj in early October.
Liberia, where the death toll is rising fastest, is struggling to cope. Many residents are panicking, in some cases casting out bodies onto the streets of Monrovia to avoid quarantine measures, officials said.
Beneath heavy rain, ambulance sirens wailed through the otherwise quiet streets of Monrovia as residents heeded a government request to stay at home for three days of fasting and prayers.
“Everyone is afraid of Ebola. You cannot tell who has Ebola or not. Ebola is not like a cut mark that you can see and run,” said Sarah Wehyee as she stocked up on food at the local market in Paynesville, an eastern suburb of Monrovia.
TROOPS DEPLOYED IN OPERATION “WHITE SHIELD”
St. Joseph’s Catholic hospital in Monrovia was shut down after the Cameroonian hospital director died from Ebola, authorities said. Six staff subsequently tested positive for the disease, including two nuns and 75-year-old Spanish priest Miguel Pajares, who is due to be repatriated by a special medical aircraft on Wednesday.
Spain’s Health Ministry denied that one of the nuns, born in Equatorial Guinea but holding Spanish nationality, had tested positive for Ebola. The other nun is Congolese.
“We hope they can evacuate us. It would be marvelous, because we know that, if they take us to Spain, at least we will be in good hands,” Pajares told CNN in Spanish this week.
More than 60 healthcare workers have died fighting the virus, a heavy blow in a region where doctors are already in chronically short supply. Two U.S. health workers from the Christian medical charity Samaritan’s Purse and missionary group SIM USA caught the virus in Monrovia and are receiving treatment in an Atlanta hospital.
The two saw their conditions improve by varying degrees in Liberia after they received an experimental drug, a representative for the charity said. Three of the world’s leading Ebola specialists urged the WHO to offer people in West Africa the chance to take experimental drugs.
A spokesman said the Liberian government would be willing to allow in-country clinical trials.
At a news conference in Washington, asked whether the United States planned to make the experimental drug available to affected African nations, U.S. President Barack Obama said he lacked enough information to give it a green light.
“We’ve got to let the science guide us and I don’t think all the information is in on whether this drug is helpful,” the president said at a news conference at the end of an African summit. “The Ebola virus both currently and in the past is controllable if you have a strong public health infrastructure in place.”
He added: “We’re focusing on the public health approach right now, but I will continue to seek information about what we’re learning about these drugs going forward.”
Ebola, a highly contagious hemorrhagic fever, kills more than half of the people who contract it. Victims suffer from fever, vomiting, diarrhea and internal and external bleeding.
Many hospitals and clinics have been forced to close across Liberia, often because health workers are afraid of contracting the virus or because of abuse by locals who think the disease is a government conspiracy.
In an effort to control the disease’s spread, Liberia has deployed the army to implement controls and isolate severely affected communities, an operation code-named “White Shield”.
The information ministry said on Wednesday that soldiers were being deployed to the rural counties of Lofa, Bong, Cape Mount and Bomi to set up checkpoints and implement tracing measures on residents suspected of contact with victims.
Neighboring Sierra Leone said it has implemented new restrictions at the airport and that it was asking passengers to take a temperature test. In the east, soldiers set up roadblocks to limit access to affected areas, MSF’s Lorenzi said.
Some major airlines, such as British Airways and Emirates [EMIRA.UL], have halted flights to affected countries, while many expatriates are leaving, officials said. “We’ve seen international workers leaving the country in numbers,” Liberia’s Finance Minister Amara Konneh told Reuters.
Randgold Resources, which mines gold in neighboring Mali and Ivory Coast, advised its workers not to travel to the affected countries.
India and Greece advised their citizens against non-essential travel to Guinea, Liberia, Sierra Leone and Nigeria and said they would take extra measures at entry ports.
- Details
- Ngwa Bertrand
- Hits: 3858
- Details
- Health
Nigeria's President Goodluck Jonathan declared a national state of emergency on Friday over the Ebola outbreak in Africa's most populous country, and he approved 1.9 billion naira (€8.6bn) of emergency funds to contain it. Nigeria has confirmed seven cases of Ebola since a man fell sick on arrival from Liberia, two of whom have died.
Several dozens of people who came into contact with the man are under surveillance.
- Details
- Ngwa Bertrand
- Hits: 2765
- Details
- Health
The death toll from the Ebola outbreak in West Africa has jumped to nearly 900 and even more with dozens of new fatalities reported in Guinea, Liberia and Sierra Leone.
The World Health Organization released new figures Monday as authorities in Nigeria reported the country's second confirmed case of Ebola -- a doctor who treated the first patient, who died July 25 in Lagos.
The World Health Organization is reporting that the total number of cases across four West African countries stands at 1,603, including 887 people who have died. A second person has been diagnosed with Ebola in Nigeria, after a Liberian-American man with the disease died in Nigeria less than two weeks ago. Eight other people are being quarantined and three are awaiting test results. The Nigerian government says it is increasing health screenings at airports and international land borders after tests confirmed over the weekend that a Nigerian doctor has Ebola. The Lagos doctor cared for Patrick Sawyer, a Nigerian-American finance consultant who traveled to Nigeria through Ghana and Togo, collapsing when he arrived in Lagos. He was immediately isolated and died from Ebola July 25. The sick doctor is currently being treated in isolation.
The Health minister Onyebuchi Chukwu told newsmen that the government is reassessing calls to close some Nigerian borders on a daily basis. "Regarding the issue of whether we should close our border: We still maintain that for now we are not doing that for a number of reasons. But if it becomes necessary we will do that,' he said.
So far the outbreak in Nigeria appears to be relatively contained, with one death and symptoms now showing in eight currently-isolated health workers that contacted Sawyer directly.
Chukwu says the body of a person discovered in a morgue last week that was suspected to have died of Ebola before he was flown into Nigeria is currently being tested for Ebola. He says Nigeria has moved to stop the import of bodies for burial from countries that have Ebola.
"They should not bring back corpses from the three countries that have the greatest number of cases,' Chukwu stressed. 'They should not bring back dead bodies. It's better that dead bodies are buried where they've had issues. Except where it is clear from the death certificate that it is not Ebola. Ebola is one of the world's most contagious diseases with up to a 90 percent death rate and it remains contagious to others after you die. Doctors attribute the current 60 percent death rate to early treatment.Humans get Ebola from handling or eating wild animals, like primates or bats, and then people spread it to others through contact with bodily fluids.And although doctors say it is not commonly spread through casual contact, officials fear that the growing number of patients and the shrinking number of aid workers in West Africa increases the threat of the disease.
US sending experts to help with Ebola effort
The U.S. Centers for Disease Control is sending 50 public health experts to help three West African nations battling Ebola.
The experts are scheduled to arrive in Guinea, Sierra Leone and Liberia by the end of the month.
Last week, the World Health Organization announced a $100 million emergency plan in conjunction with the three affected countries that includes a strengthening of control and response measures. A WHO spokesman said some 600 specialists would be needed to carry out the plan.
More than 2,000 volunteers from the International Red Cross Federation have been working in all three countries since the outbreak began.
American doctor receiving treatment in Georgia
Meanwhile, an American doctor who contracted the virus while treating patients in Liberia returned home Saturday and is being treated in isolation at Emory University Hospital in Atlanta, Georgia.
The Christian charity Samaritan's Purse says Dr. Kent Brantly received a dose of an experimental serum before leaving Liberia, and also received blood from a 14-year-old boy who had survived Ebola under his care.
Another U.S. missionary who contracted the disease in Liberia, Nancy Writebol, is expected to fly on Tuesday to Atlanta. She will also be treated at Emory.
No cure, vaccine under development
While there is currently no cure or vaccine for Ebola, Dr. Anthony Fauci of the National Institutes of Health said a vaccine is being developed and could soon go to trial. Fauci spoke Monday on the TV program CBS This Morning.
Tom Frieden, the head of the Centers for Disease Control, says a widespread outbreak of Ebola in the U.S. not likely, citing better infection controls at American hospitals and more cautious burial procedures than in Africa.
- Details
- Ngwa Bertrand
- Hits: 3224
- Details
- Health
Bushmeat - from bats to antelopes, squirrels, porcupines and monkeys - has long held pride of place on family menus in Cameroon, whether stewed, smoked or roasted.But an outbreak of the deadly Ebola fever in West Africa has rekindled concerns about the health risks of age-old African hunting and eating traditions that bring humans into close contact with wild forest animals.
If you are currently looking for bush meat in the country's capital city, go right now to the busy Nkolndongo Market which is characterised by the display of fresh and smoked bush meat. Vendors there sell snakes as tall as a human being, striped civets, antelopes, rabbit, hind, hedgehog, pangolin and porcupines with spiky fur and lots of different kinds of monkeys.
In spite of the current ban in the hunting of all species of animals due to their reproduction period, traders in bush meat do not seem bothered by the fact that they are into a forbidden trade. Yesterday July 29, 2014 Cameroon Tribune (CT) visited the bush meat market at the Nkolndongo neighbourhood in Yaounde. Besides the enormous display of smoked bush meat of all sorts, the number of fresh meat available outweighs that which has been smoked.
While CT reporters went round the market showing interest in buying fresh pangolin, over 10 traders in pangolin, mostly women rushed forward with newly killed or life pangolin at different cost. Some of the pangolin sold at FCFA 4000 while others went up to FCFA 15,000.
But the surprising thing is that when CT reporter asked to know where the meat comes from, and whether it's legal or illegal, there was no luck in this as most of the traders went back to the corners they have placed their bush meat. Nobody was interested in answering any question from CT reporters other than the interest to sell at a profitable rate.
As CT reporters looked on in dismay, one woman, speaking from her corner said, "people come and sell it to us; I do not know where they come from. They just come from the bush". From all indication, the lady does not even know if the animals she sells are protected species. She is interested in selling bush meat to make ends meet. "I am waiting for the day when I might have a problem with the authorities," the lady added.
Traders in bush meat are not hiding in what they are doing, although there is a current announcement from the Ministry of Forestry and Wildlife forbidding the hunting of all species of animal during this time regarded as their reproduction period. One of the guys at the Nkolndongo Market, specialised in cleaning animals after purchase said he was willing to discuss with the CT team in a private zone at a cost. When asked if he was aware of the fact that trading in all sort of animals was forbidden during this period, he vehemently said yes.
When asked why they are in such a business, he told CT reporters he cannot betray his mates unless he was given FCFA 5000. There are signs that people are making brisk business from bush meat and this is really a problem to forest guards as the hunting pressure keeps pressing on authorities who know that the animals need protection.
- Details
- Ngwa Bertrand
- Hits: 3530
Flourish Doctor Article Count: 3
Meet Your Coach Dr. Joyce Akwe ... With a master's in public health and a medical doctor specialized in internal medicine with a focus on hospital medicine.
Dr. Joyce Akwe is the Chief of Hospital Medicine at the Atlanta VA Health Care System (Atlanta VAHCS), an Associate Professor of Medicine at Emory University School of Medicine and an Adjunct Faculty with Morehouse School of Medicine in Atlanta GA.
After Medical school Dr. Akwe worked for the World Health Organization and then decided to go back to clinical medicine. She completed her internal medicine residency and chief resident year at Morehouse School of Medicine. After that, she joined the Atlanta Veterans VAHCS Hospital Medicine team and has been caring for our nation’s Veterans since then.
Dr. Akwe has built her career in service and leadership at the Atlanta VA HealthCare System, but her influence has extended beyond your work at the Atlanta VA, Emory University, and Morehouse School of Medicine. She has mentored multiple young physicians and continuous to do so. She has previously been recognized by the Chapter for her community service (2010), teaching (as recipient of the 2014 J Willis Hurst Outstanding Bedside Teaching Award), and for your inspirational leadership to younger physicians (as recipient of the 2018 Mark Silverman Award). The Walter J. Moore Leadership Award is another laudable milestone in your car
Dr. Akwe teaches medical students, interns and residents. She particularly enjoys bedside teaching and Quality improvement in Health care which is aimed at improving patient care. Dr. Akwe received the distinguished physician award from Emory University School of medicine and the Nanette Wenger Award for leadership. She has published multiple papers on health care topics.
Local News
- Details
- Society

Kribi II: Man Caught Allegedly Abusing Child
- News Team
- 14.Sep.2025
- Details
- Society

Back to School 2025/2026 – Spotlight on Bamenda & Nkambe
- News Team
- 08.Sep.2025
- Details
- Society

Cameroon 2025: From Kamto to Biya: Longue Longue’s political flip shocks supporters
- News Team
- 08.Sep.2025
- Details
- Society

Meiganga bus crash spotlights Cameroon’s road safety crisis
- News Team
- 05.Sep.2025
EditorialView all
- Details
- Editorial
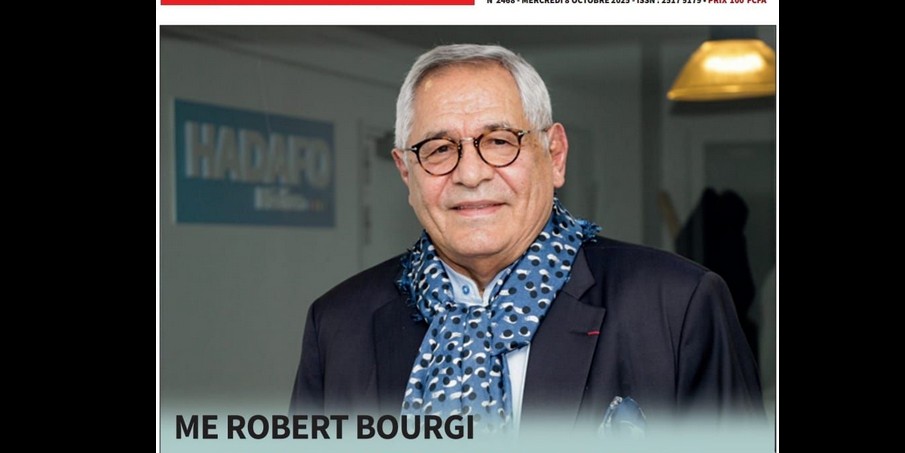
Robert Bourgi Turns on Paul Biya, Declares Him a Political Corpse
- News Team
- 10.Oct.2025
- Details
- Editorial

Heat in Maroua: What Biya’s Return Really Signals
- News Team
- 08.Oct.2025
- Details
- Editorial

Issa Tchiroma: Charles Mambo’s “Change Candidate” for Cameroon
- News Team
- 11.Sep.2025
- Details
- Editorial





